Maitreyi has been working on mental health in prisons from different entry points, for the past 10 years. She has conducted empirical research, and has provided legal representation to death row prisoners, many of whom are struggling with a variety of mental health concerns. Her first comprehensive engagement with the issue was with Project 39A’s report, Deathworthy, which she led.
Through her recent work on a public interest litigation, Maitreyi’s understanding of mental health in prisons saw a shift. What happens when care turns paternalistic? Can the promise of freedom be used as a tool to negotiate/manipulate? Are our imagined alternatives to this system any better? This interview is an attempt to make sense of some of these questions.
TTE: As a lawyer, what drew you to mental health in prisons, especially that of death row prisoners?
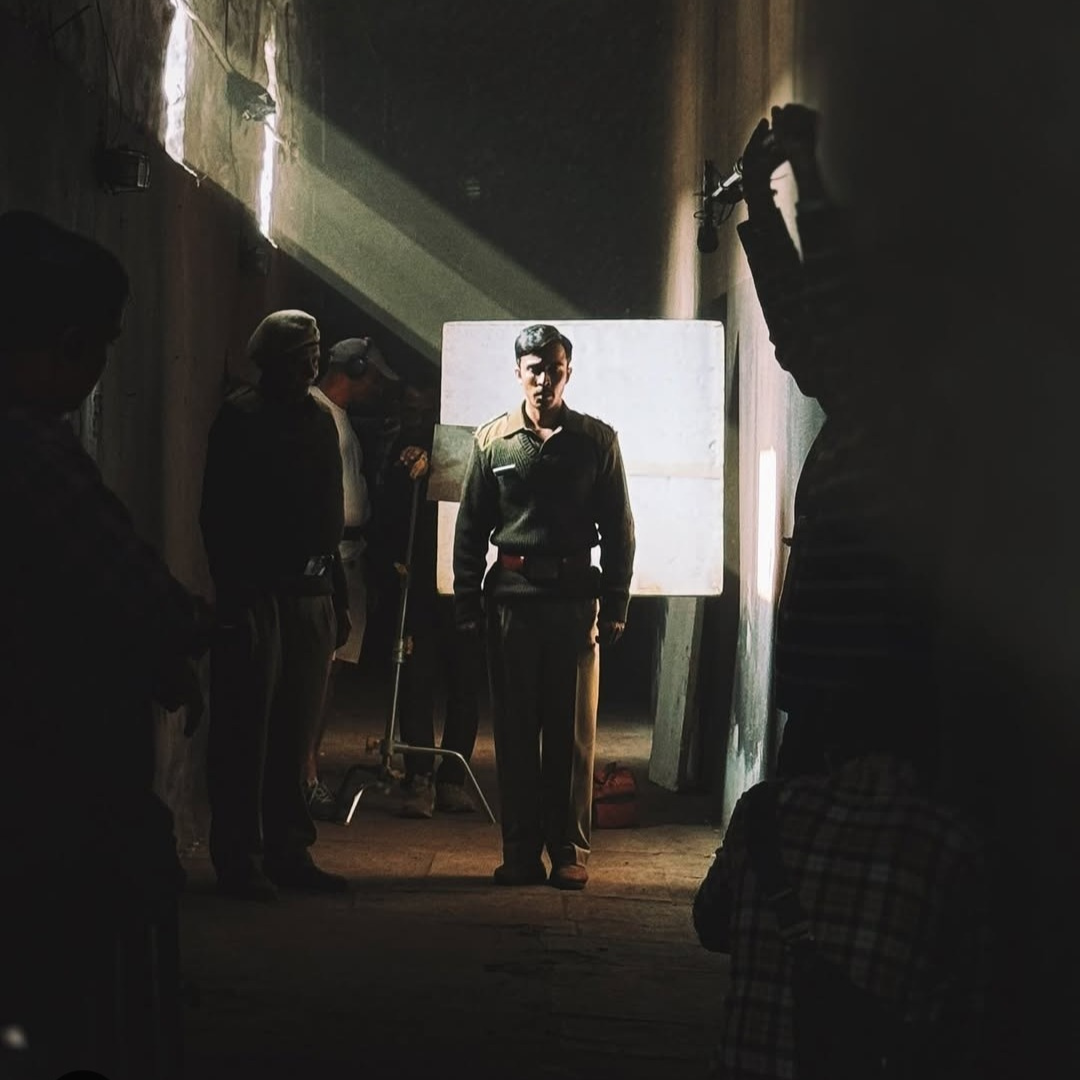
Maitreyi: The reason I’m interested in prison mental health is because being literally walled-off spaces, prisons are simultaneously part of our society and alien to it; they are contradictory ideas.
As a space, prison enforces loneliness and is helmed in by suspicion, so it’s automatically a space that is antithetical to happiness.
Of course, you’ll find prisoners laughing and sharing stories inside prison, so it’s not a permanently desolate space where everyone is always in despair through the day and years. It’s interesting, my urge to make this qualification. I also feel the need to communicate the humanness of individuals occupying a space like prison (as if the fact of humanness is surprising in prison).
But back to my initial point: I think prisons are very much the walls that surround them. It’s very hard to get anything inside them — including necessities like health service and education — the prison is an ecosystem that doesn’t interact with other ecosystems. In different ways it’s stuck in time, but people who come in and go out are constantly changing. So again, there are a lot of contradictions that haven’t resolved themselves in any coherent manner.
In providing legal representation, I’ve had the opportunity to think through the implications of mental health concerns for the law (if any), and the duty of care owed by the State to death row prisoners with mental health concerns/disabilities. (From hereon, I will use the phrase ‘mental disabilities’ for convenience and to indicate diagnosis).
The most recent work that I did arose out of an ongoing public interest litigation, and for this, my colleagues and I at Project 39A, as well as field researchers, interviewed undertrial and convicted prisoners with diagnosed mental disabilities. We also interviewed prison and welfare officers, prison inmates and some mental health professionals.
The aim of this research was to enquire into prison mental health care and treatment infrastructure, and to think through ways of making it better and more effective.
Prior to this, I led Project 39A’s report Deathworthy, which looked at the death penalty (the law, experience of being on death row, and the lives of death row prisoners from a mental health lens). We interviewed 88 death row prisoners and their families to understand and identify (a) the prisoners’ mental health concerns (illness, disability, distress — whatever framework one may want to use), (b) how mental health concerns may be impacting and getting impacted by different individual, familial and structural factors for those on death row, and (c) the mental health impact of being sentenced to death.
Personally, with this study there was a shift in the way I heard and made sense of the stories I came across: how and what I was observing in the field, and even my understanding of fundamentals, like what consent may mean for a category of persons often deemed incapable of giving or refusing consent.
TTE: When you wrote about a feminist way of looking at crime for TTE, you foregrounded ethics of care as a framework to do so. How does care inform a research framework for mental health in prisons?
Maitreyi: In prisons, the idea of care is very tightly intertwined with security.
For instance, care is either competing with security, or security is seen as care
And care is often subservient to security because despite what our prison manuals may say about prisons being reformatory spaces, they are, in fact, places with centuries-old history of security, surveillance and suspicion in their bones.
Institutional memories, culture and conventions have been passed down through the years and the version of care that seems to have developed is one that needs to continuously be fenced-in by security (as opposed to safety).
When it comes to prisoners with mental disabilities, the security-as-care model is even more prevalent. The overlap of identities — prisoner and mentally disabled — seems to produce an interesting state of affairs, where prisoners with mental disabilities are simultaneously dangerous and pitiful. Therefore, prisoners with mental disabilities are only receptacles of care.
For me, this is the crucial difference between care and ethics of care. The former may very well be aligned with treating the object of care as passive, but the latter is quite averse to treating care as simply flowing from the able to the disabled.
Because of its focus on context, relationality and interdependence, the ethics of care requires that no one be treated as passive beings.
I think one of its prerequisites and continuing values is the idea of empowerment.
A practice centred on ethics of care will require that prisoners with mental disabilities be seen neither as dangerous nor pitiful, but rather as individuals who require a certain kind of care and who are active participants in that care (as well as active participants in general).
This, in turn, would require creating necessary conditions to enable that active participation. These conditions, however, are absent and assumed to be non-existent/non-essential in the treatment of prisoners with mental disabilities. For instance, I’ve come across instances where prisoners with mental disabilities are, by default, sequestered in a ‘psychiatric ward’ for months and years with no opportunity to either interact with the general prison population, or participate in prison life in a broader sense.
Often, the logic is that the person may become violent/aggressive or that the ability to be participative no longer exists in them — just by virtue of being diagnosed with a mental disability. Even in this sequestered existence, little conversation — other than checking whether they have taken their medicines, or taken a bath, or eaten their meals — occurs.
They are seen and treated as less than whole.
One of the most important elements of mental health treatment is helping the person get reacquainted with the confidence and skill to interact with the world in a manner that feels safe. I say this because as someone who has accessed mental health treatment, medicines were an important but only a small part of my treatment. A large part of it was being taught the tools to trust myself again and be in (sometimes confident, sometimes timid but) constant negotiation with myself and the world around me. I see access to such tools, choice, and opportunities as essential to mental health treatment, which uses the ethics of care as a central framework.
TTE: Did looking at the prison structure from a mental health perspective give you new insights about the structure itself?
Maitreyi: That prisons are debilitating and not conducive to mental well-being is well known, and, unfortunately, well accepted. Overcrowding, poor hygiene, poor quality food — the structural and systemic realities of the prison itself are known to lead to mental ill-health overall, including for prisoners who are not under active mental healthcare. I have yet to come across anyone for whom prison has been healthy, uplifting and empowering. If prisons are meant to be reformatory and rehabilitative spaces, they are failing to become that space.
It is also true that for many who need mental health support, prisons are the first time they may have a chance to access that support.
I find it seriously concerning that prisons are failing to provide even that. Yes, in many (not all) prisons, prisoners may get identified as needing support — but that support is almost punitive, ineffective, and in many ways, false.
Using mental health as the primary lens helps my inquiry go deeper and focus on formal and (crucially) informal structures and interactions, as well as intangible and unspoken approaches.
Prison manuals, for instance, instruct that if a prisoner has a mental illness one must check for malingering (which means to check that the prisoner isn’t feigning symptoms). Hence, suspicion is already playing a role. I highlight this because it’s always struck me as curious that checking for malingering is such an explicit directive for mental health in prison (and the criminal justice system). Ensuring that the symptoms are being accurately reported for their presence and intensity is a necessary part of mental healthcare (and even physical healthcare), regardless of the setting. But, in prisons, it becomes an explicit directive.
To give an instance of problematic informal interactions, prisoners who may be refusing to take psychiatric medication are often told that if they take the medication they will be released soon, even though that’s not going to happen.
The promise of freedom/ being with family is used as a tool of negotiation.
It seems almost cruel to dangle that promise to someone desperate to be with their family, when you know it’s not going to be fulfilled. The person may take their medication everyday while waiting for this promise to be fulfilled, but it won’t be fulfilled because in reality, the family may have abandoned them and the legal process may not even allow for a release like this.
Again, often the sentiment and intention is ‘at least they will take their medication’, but the breakdown in trust it creates is really counterproductive, including from a recovery perspective. The constant cycle of hope and utter disappointment that the person who is trusting such a statement goes through, is surely problematic, even if it’s not being expressed.
TTE: You mentioned earlier that something shifted for you as a researcher during this study? What was that?
Maitreyi: The challenging experiences I had overlap with the ones through which I have been able to learn the most — in terms of meaning-making and imagining what mental healthcare could look like.
I once met a female prisoner who was on very strong medication for schizophrenia (if I remember her diagnosis correctly). I needed to take her consent to talk to me (as someone who wasn’t talking to her for legal representation, but for research). From the get go, she asked if my colleagues and I had come to take her home. We had to say no; we had come to just talk to her and was she, regardless, interested in talking to us? This, itself, creates certain kinds of problems in terms of research ethics, because I couldn’t be sure she understood that we weren’t there for her release. But she said she was happy to talk to us.
I was very conflicted about whether to continue talking to her, but she seemed eager to talk so we tried engaging in a conversation with great internal conflict. But we did abandon the research enquiry and thought it best to see where the conversation went. And did she have a rich inner life!
Had I stuck to my initial discomfort, I would have never had an opportunity to be a party to her life.
I asked her about the bangles she was wearing and she excitedly told us about her daughter. She told us about her married life, and did sing a song or two about a peacock and the flower madhu malti. To me, it seemed like she had a world inside her that to her, was legitimate.
The enquiry about the legal process would have given me some answers (mostly in their absence), but they would have told me nothing about her. She was fond of sweets, but because of her medication and ensuing complications, she couldn’t eat too much of them so I got to know that. I got to know that she was really fond of her long hair which had now been cut short, and she was in distress about that. She liked wearing nice clothes and feeling pretty. She liked talking and singing. I would’ve missed out on her life had I stuck to my pedantic inquiry. I would’ve missed out on wondering whether that’s one way to think about mental healthcare.
Listening to stories and engaging with them from the narrator’s point of view is sometimes more important and useful than asking questions about what we as interlocutors think is important.
Whether it happened or didn’t is sometimes besides the point; that someone is listening and engaging with a story that another wants to tell is important. I was neither there to interrogate her nor to aid in her recovery, but I did realise that there is a benefit to talking to people just for the sake of talking. It needn’t be for a purpose. For me, it highlighted the importance of everyday random conversations that we have with family, friends, colleagues and strangers. Not everything need be for the sake of eliciting information or towards a ‘purpose’ or with an ‘aim’.
With many other prisoners, this pattern repeated. Their rich stories were difficult for us as outsiders to understand, but they had an internal logic.
And even if there was no internal logic, what if stories were of fundamental importance?
Maybe if we didn’t mock them for those stories, took them as bizarre and therefore useless, or discard them as not fit for ‘purpose’, we would get somewhere.
Maybe, it would mean recovery on their own terms.
TTE: People living with mental disabilities are perceived as ‘deviant’ in society. In prison, prisoners by virtue of being ‘criminals’ are considered ‘deviant’. What implications then, does this overlap of identities have on their personhood?
Maitreyi: The overlapping identities definitely create an interesting space where a person is both dangerous and pitiful at the same time. But that’s not the only dynamic. Persons with mental disabilities are seen as odd people with strange behaviours and even stranger minds.
I wonder whether they are seen as people with mysterious minds — almost mythical.
Yet, because they have strange minds and ‘odd’ behaviours, they could also be dangerous and unpredictable (or so the perception goes). In cases of a person with mental disability who is also a prisoner, particularly when they may have been convicted or accused of violent offences, the stigma is compounded because they have, in a way, proved their dangerousness.
There is yet another interesting dynamic. Persons with mental disabilities are often laughed at because of their strangeness, but among the prison inmates it translates as someone you can laugh at but must at the same time be slightly scared of. Many of the prisoners with mental disabilities seemed to exist in liminal spaces where they are making sense of their external and internal worlds. Due to the overlapping deviant identities, I wonder whether these worlds collide, run parallel, opposite to each other or are enmeshed, because the world that is external to them seems to have rejected them — both in their presumed dangerousness and strangeness — and therefore, has no interest in the internal lives of prisoners with mental disabilities. Their internal worlds have rarely been opened up to let the external world in.
There’s an uncertainty that exists around and about prisoners with mental disability, which then makes their sequestration a ‘safe option’.
But this results in extremely reduced opportunities for prisoners to engage in prison life, to roam around, to seek spaces that they like et cetera, which in turn seriously hinders their recovery. It becomes a self-fulfilling prophecy.
What is clear is that the manner in which inmate-caregivers, officers and others interact with prisoners with disabilities is often dismissiveness, amusement, violence, othering, derision or pity. I think it’s because prisoners with mental disabilities are not seen as whole. Due to the othering and rejection, large parts of their lives go unaccounted for and unengaged with. For the prisoner whose hair was chopped off against her wishes, it was a traumatic experience because she lost a part of herself — a part that she was proud of. But this will seem like a second-order concern to anyone who hasn’t engaged with her.
The mistrust and fear start to dominate what should ideally be an environment of care. In fact, formal processes meant to ensure care are often looked at from a point of view of bureaucratic compliance, so that the prison doesn’t get blamed for any harm. Escape from blame many times becomes the primary lens rather than care, which obviously then has an impact on the quality, integrity and depth with which the prison understands particular things. It may be formal compliance with certain rules, but it’s not meaningful.
TTE: How much of the prison-society continuum comes into play here? Did you find any ruptures/new entry points for intervention?
Maitreyi: The tropes of persons with mental disabilities being dangerous and unable to participate in public and private life are very much alive in prisons as well. The tendency to speak for persons with disabilities and the paternal/benign dismissal of their needs, wants, and choices is much more intensified in prison.
But what I found interesting was also the lack of shame.
Many families are ashamed of having a member with mental disability and often hide them away. But in prisons, that shame doesn’t exist, and I think that could be a very powerful site for change, although currently the space left by an absence of shame is fully occupied by paternalistic care.
In society, the attitude towards persons with mental disabilities is often quietly condescending. What I mean is, if a person with mental disability has, let’s say, painted a piece of art, there’s an automatic need to be impressed or to praise. If I were to voice my opinion that the painting isn’t nice, I’m likely to be judged poorly. So, too, in prisons, where often those in authority will treat prisoners with mental disabilities like infants. Many, in fact, see it as a good thing. But it’s not because (a) it assumes a false equivalence between children and the wealth of experience that adults (including adults with mental disabilities) accumulate, and (b) it assumes that those with disabilities will not be able to deal with the daily burdens and joys of life.
On the diametrically opposite extreme is the use of violence; often because the person with mental disability is not behaving like an infant should. They may resist, demand, object, have a different view, and may not accept care as it is being given. That, I think, often becomes a sore point for caregivers to come to terms with and leads to obvious and insidious forms of violence, like mixing medicine in meals in order to fool the person into taking medication. It’s the same in prison, and might just be worse, because the lack of capacity is an assumption present among all stakeholders in the criminal justice system.
Hence, coercive care is omnipresent and care then always has the latent potential to become violent in an instant.
TTE: What made you most uncomfortable during this study?
Maitreyi: The loneliness and abandonment that I witnessed makes me intensely uncomfortable. Often prisoners who are on very high doses of psychiatric medicines have lost track of the decades that they have spent in prison, they have lost track of what’s happening in their legal case, they have lost track that their family no longer wants them. Prisoners expectantly looking at us as if we’re going to rescue them, or excitedly asking us whether we’ve come to take them to their family is one of the hardest things I have experienced in prison research.
But the most disconcerting is the systematic way in which a person is made irrelevant.
When you see medical prescriptions for mental disabilities such as schizophrenia, you might come across phrases like ‘irrelevant talk’ or ‘smiling inappropriately’, which is a psychiatric shorthand to indicate some constitutive symptoms of schizophrenia. This psychiatric shorthand, however, doesn’t provide any indication about the content of the irrelevant talk or what prompts the person to smile, even if inappropriately. It doesn’t allow for any meaning-making and instead of being a description of the symptom, it becomes a description of the person itself.
So, prisoners with mental disabilities become the symptom itself — irrelevant and inappropriate.
I once worked on a case where the prisoner would talk of a friend who spoke to him through the radio. It was an imaginary person he was talking about, but very real to him. But that voice would also help him. He, in fact, mentioned that often this imaginary friend would urge him to do basic tasks like taking a bath and eating his meals. However, not even once was this mentioned in any of his prison medical records. It’s the same in other prisons, where prisoners with mental disabilities, particularly those who may be in psychiatric wards, are provided medication. Anything else they may say —if it doesn’t match with other people’s reality — is considered irrelevant and dismissed.
In one of the prisons I visited, I felt a sense of great frustration about why no one was listening to the stories these prisoners had to tell. I’ve tried looking for answers about why it affected me so much. Currently my theory is that perhaps when I was really ill I had a fear that people would forget me or that no one would see me, even though I was there.
The fear of being made invisible and forgotten.

It made me remember how sometimes, during those days, my mind would feel very fragmented. It felt like having to gather these shattered pieces and put them back together. But they won’t fit, and you don’t know how to ask for help — but you keep trying, the panic rises, you can’t breathe, and finally it chokes you. So, you swallow back your effort and just sit —sometimes you cry, sometimes you sleep tired and defeated. It’s a feeling that scares me. That’s what I can sense sometimes. That’s the kind of loneliness and abandonment I’m talking about.
TTE: What are some of the measures you are suggesting that could bring some humanity to the prison system vis-a-vis prisoners with mental disabilities?
Maitreyi: There needs to be an institutional shift towards recognising that prisoners with mental disabilities are full agents of their own lives. I’m not saying that support and care are not required — but they cannot become oppressive and should not be subsumed into the rhetoric of administrative convenience. At the very least, the kind of mental health treatment and care that prisoners are provided should follow contemporary clinical ethics.
Mutual trust is a prerequisite for effective mental healthcare care but little effort is made to foster an environment conducive to trust.
Lack of proper training to prisoner-caregivers, prison and welfare officers often results in day-to-day practices that may feel right to them, but are in fact problematic, harmful, and counterproductive.
For example, I’ve often come across instances where if a prisoner with mental disability is getting aggressive, they will be handcuffed for hours together, be physically restrained or injected with a sedative. This happens because there’s no training provided in de-escalation techniques. Handcuffing or sedating a prisoner to prevent aggression is an institution-based measure, not an evidence-based care technique, and of course, in the long run it’s going to be harmful because it is, to say the least, violent.
Basic requirements of care such as informing prisoners of their diagnosis, entering into a conversation of risk-benefit regarding treatment, explaining the side-effects, (or even keeping a track of them), or taking these concerns seriously are all severely lacking in most prisons. These are fundamentals of care, but most prisons don’t consider it relevant, or sometimes even feasible. Simple things like a copy of the prescription or the health records aren’t available to prisoners. Prisons don’t do it for sometimes very puzzling reasons, such as ‘the prisoner will lose it’ or that ‘the prisoner will use it to their advantage to get released’. The thing is, a simple thing like a piece of paper — that tells a person what they are being treated for, what medicines they’re taking, what each medicine is for — is a record that can help a person with mental disability make sense of what’s happening to them and keep them grounded. And it can help them find more information about their illness as well.
It’s just a piece of paper but it’s an important record of a person’s life.
TTE: What about the resource constraint most prisons work under?
Maitreyi: Well, then, let’s put in more resources and use the resources that already exist more effectively. For instance, the one resource that is not lacking in prison are prison inmates. Prisons rely on inmates for a variety of tasks in the day-to-day functioning of the prison — cooking, cleaning, maintaining the garden, working in prison officers’ offices, and providing care to other inmates. A lot of problems regarding insufficient human resources for caregiving, and even preventing escalation of mental health issues can be solved if prisoners who are interested are provided proper training in caregiving — such as in the fields of psychological first-aid, identifying distress, peer counselling or mental health nursing.
Effective peer counselling is likely to reduce overall distress in prisons. In fact, peer counselling is suggested as a minimum standard for prison mental healthcare under the Mental Healthcare Act Rules of 2018 but that’s not been implemented. Though they are overly broad and provide little specific guidance on what prison mental healthcare should look like, prisons haven’t implemented that either.
Currently, prison mental health is about treating individuals and no thought has been given to structural and systemic concerns. Courts have often said that prisoners with mental disabilities should not be in prison, with an assumption that families will support the prisoner. But many prisoners with mental disabilities have been abandoned by their family, so where will they go?
We don’t have half-way homes and residential facilities that are uniformly connected to prisons.
Once a prisoner with mental disabilities is released, how are the State bodies going to ensure that care and treatment continues to be provided to them? These structures need to be put in place and strengthened.
Ministries such as those of health, social welfare, education, labour should be integrated into prisons as an institutional measure, because for better mental health, structural conditions need to be addressed. Better integration will help in providing effective care to prisoners with mental disabilities not only in prison, but also outside of prison, once they are released. It must be pointed out that government rehabilitation centres are no better and are often worse than prisons. The recent news about Delhi’s Asha Kiran home speaks to the appalling conditions in which the residents are kept. News like this makes me conflicted that prisoners with mental disabilities might be better off in prisons if they don’t have families, because the alternative doesn’t seem to be any better.
Even if prisoners were to be released, the understanding of mental healthcare in prisons is such that efforts to reacquaint prisoners with mental disabilities with skills required for independent living are not considered part of it. So, upon release they may have to be detained in halfway homes for long periods of time. This also becomes a barrier for release, because after spending decades in prison, they become reliant on someone caring for them. They aren’t being helped with life skills because they can neither access education nor vocational training if they are in psychiatric wards.
So, an important question that needs to be answered is about the goal of providing care.
The goal of mental healthcare has to be recovery and empowerment. I can almost hear the protest about empowering prisoners with mental disabilities, but it is key to recovery.
A common response to agency, autonomy, consent and empowerment of prisoners with mental disabilities is: but what about people who ‘have a break with reality’. I suspect this question arises because we automatically think about prisoners with mental disabilities who have spent years in prison under medication (in some prisons even access to medication is not easy) without any psychosocial support. I think providing necessary and effective psychosocial support will make the question and this assumption largely redundant.
I also think we don’t pay sufficient attention to preventive measures. Prisoners are not a homogenous group and their mental health needs therefore are not going to be homogenous.
For instance, the mental health support needs of undertrial prisoners, geriatric prisoners and female prisoners are going to be different.
Maitreyi Misra heads the work on death penalty mitigation as well as mental health and criminal justice at Project 39A, a criminal justice program at the National Law University, Delhi. She is the lead author of Project 39A’s report, Deathworthy: A Mental Health Perspective of the Death Penalty.